|
I have a bone to pick with expectations. I first learnt about them on a student exchange trip to France at the age of 17. It was meant to be “amazing”, a “once in a lifetime experience”. Instead it was lonely and difficult. I found myself in a world where I could not express myself and as a result became an outsider, that awkward person that hangs on to groups of people without contributing. I became depressed and felt guilty for squandering this “amazing” experience with my own genuine feelings. I was so disappointed and let down by my experience and felt the blame lay squarely on my unrealistic expectations. This spurred a realisation for me. Expectations can ruin an experience. Not once in the lead-up to my 2 months abroad did anyone say to me: “you’ll feel really lost”. Instead it was “you’ll find yourself”. Well, I found more of my physical self as I made a daily trip to the patisserie to fill my emotional void with sugar coated almond croissants. But unfortunately, I had never felt more insignificant. Yum! Image by Faruk Ates Looking back, I still think it was a valuable experience, but it should have been just that…an experience, not “the time of my life”. I think that actually goes for most major events in life. I had a similar experience following the birth of my first child, Lily. The most common question I was asked during my pregnancy was: “Are you excited?” After hearing this for the 20th time, my response was reactionary and immediate, I would break out the big smile, nod profusely and explain I couldn’t wait. And it was the truth. But the effect of this question was like hypnosis for me. It solidified my subconscious thinking that parenthood was meant to be, and going to be ‘exciting’. Even if I may have read a chapter on settling, or listened to the antenatal session on juggling time in the post-natal period, these concepts were abstract and hard to tangibly imagine. The overwhelming emphasis from my world was that this was going to be the most exciting and rewarding journey of my life. Then, diagnosed with post-natal depression when Lily was 6 months old, I was perplexed. This was meant to be exciting and rewarding. Why was I finding it so difficult? How is it, that millions of women have done this mothering caper the world over, and I feel it is beating me? I was young, healthy, fit, and educated. I had read the books and attended the classes. At my kinder graduation aged 5, my teacher proudly announced I wanted to be a mum when I grew up. BRING IT ON!! The reality…you all know it, turn on the broken record. Tired beyond all scope of possible imaginings, feelings of defeatism as a tiny person up-ends your life and makes you feel inadequate, body changing issues, a feeling of distance with your partner, watching your friends go overseas and earn money and attend trendy wine tasting events. I was expecting this: But I was experiencing this: Image: shoeboxblog.com I thought there was something wrong with me. Now I know, there wasn’t. My expectations were just so far from reality that I had lost before I had even begun.
I tried to keep up the performance of being on top of everything and “happy”. It was EXHAUSTING. But why did I do it? I’m still not entirely sure. Maybe because I didn’t want to let down everyone who was telling me how happy I should be. Maybe because people don’t want to visit you when your a vomit-stained, un-washed, teary mess who keeps falling asleep. Maybe because I thought I’d fool myself if I kept on the hamster wheel. Did it work? Yeah, maybe. Sort of. Not really. What did work? Talking. Well for me anyway. Mothers’ group was brilliant. 8 other mum’s right there in the trenches with me, sleep deprived, angry at our husbands, feeling like slaves to our 6 months olds. It was gold. We used to open a bottle of wine at 12.30PM and get it all off our chests. Then I had to talk to a psychologist for a bit as well. Similar issues, less wine and more expensive; but also very helpful. Should 1 in 7 mums experience post-natal depression? It seems wrong to me. So, I find myself asking, what are we doing as a culture, as a society that makes this feeling of defeatism and sadness so profoundly common in new mums? Unrealistic expectations are playing their part. Unrealistic expectations of happiness, of fulfilment, of love, of connection with your partner, of physical recovery. And unrealistic expectations and understanding of the enormity and loneliness of the mother workload. So, as a community can we moderate this expectation? I think we can. It’s not about bringing all pregnant women down and telling them depressing stories about motherhood. But let’s just say it how it is. There are high’s and there are low’s. Let’s ask open ended questions to pregnant or new mums such as “How are you feeling about becoming a mum?” to allow them to express themselves, rather than ramming pre-packaged emotions into their psyche. None of this is to say it’s not worth it. And for goodness sake, share your lovely stories about your children too. But don’t sugar coat parenthood. Don’t watch too many nappy ads that make being a mother look like running through an immaculate house in white pants while your perfectly clean child giggles constantly. Sure, there is the odd moment like that (FYI: you’re mad if you wear white anything as a mum, and my house has never been immaculate since becoming a parent) but the bare bottomed giggles and the cuddles do happen, and are awesome! As a community and society, let’s help to put expecting parents in a frame of mind that acknowledges the road into parenthood not as “the time of your life” but for what it is, an experience.
3 Comments
Do you wee more than every 2 hours? Do you wake up overnight to wee? Do you make sure you go to the toilet before you leave the house? Do you rush to the toilet as soon as you get in the door?
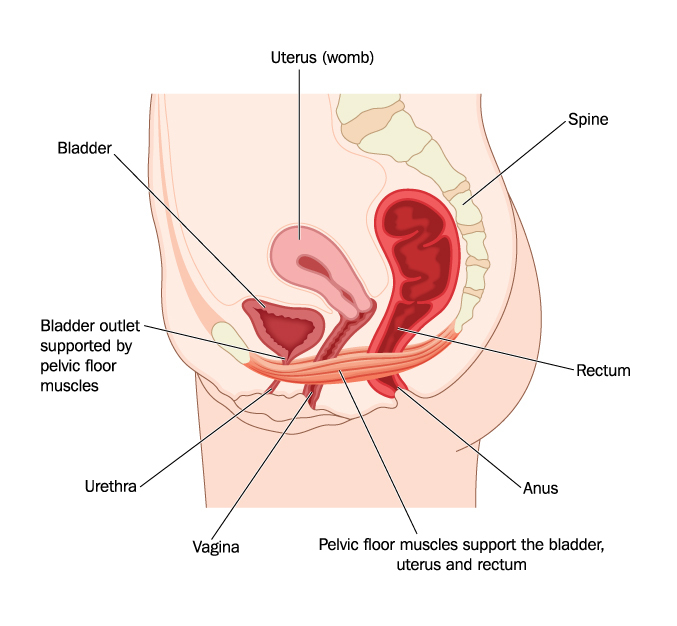
If you answered yes to any of the above questions, you are not using your bladder correctly, and you could be setting yourself up for conditions such as:
The bladder’s job is to fill, store and then empty urine. The bladder is a muscle, called the detrusor muscle. Which means it’s really good at stretching, then forcefully contracting and rebounding to it’s normal shape. And it does this over and over and over, every day of our lives. Within the wall of the bladder, there are baroreceptors, or ‘pressure receptors’ that feedback information to our brain about how the bladder is filling. Once these messages get loud enough, they come to our conscious attention, and we get the urge to go to the toilet. Once on the toilet, our brain sends a message to the bladder to contract, and the bladder muscle squeezes all our urine out. Sounds simple right? And it can be. But the bladder muscle, like every muscle in our body, contracts best within a certain range of motion. Or, in the case of the bladder, within a certain volume of urine. So, why do we care if our bladder is, or isn’t contracting at it’s best? If the bladder is not filled enough, then the detrusor muscle is unable to generate sufficient force to expel all the urine, and we can experience; poor urine flow, increased post-void residual (the amount of urine left in the bladder after emptying), urinary frequency, and increased risk of urinary tract infections. Additionally, over time, if the bladder is never allowed to fill up and stretch, the detrusor muscle becomes stiff and can become unable to hold decent urine volumes. This can progress to symptoms such as urinary urgency, urinary frequency, nocturia (waking more than once per night to urinate), and urinary urge incontinence. Now, don’t get too carried away on the big wee’s, bigger is not always better. If you repeatedly over-stretch your bladder muscle, you end up with lazy pressure receptors that forget to send your brain the message that your bladder is filling. Also, your bladder ends up looking like a deflated balloon and this also can result in poor urine flow, poor emptying and urinary urgency. So, hopefully now you are asking “What is this magic volume that I need to be wee-ing at every toilet stop?” Drum roll please…..Optimal bladder habits are as follows: 250-500mls per wee 5-6 wee’s per day 0-1 wee per night. So, how do you find out if this is what you are doing? Grab yourself a measuring device (preferably a dedicated one you have purchased for the task, and not the kitchen measuring cup), measure and write down your wee’s for at least a 24hour period. If you fall within the above range, give yourself a pat on the back (or bladder) and move on. If not, make the time to speak to a continence professional such as a urologist, continence physiotherapist or continence nurse and find out what is causing your less than optimal bladder habits, and how to fix them. Unfortunately, we know that poor bladder habits or urinary symptoms such as urgency, frequency and incontinence get worse over time unless they are treated. So seek treatment sooner rather than later. She came from my being. Started as a seed, always there. Never apart. Her number was chosen, she won and thrived; My bread was her bread, my lungs, her air. She was me. There was no divide. My rhythm was her lullaby. We became an alien, a two headed, strong willed force of nature. She came with a purpose, perfect from the start. She breathed her own oxygen and her blood pumped red. I didn’t think twice when they cut her physical bond to me. It didn’t even bleed a tear. We smiled. Why didn’t I mourn that more? She did not recognise herself, rather knew herself only in relation to me. Without my body, my scent, my sounds; she was lost. My milk sustained and nourished her. She grew fat on it. She was physically, completely a product of my body. I was her world. It came with responsibilities; some of which were terrifically, physically, emotionally challenging. Others that were utter gluttony in their delight. And all she wanted was me, we were so wrapped in each other, We may as well have been one and the same. And we were. She took food from a spoon and I mourned a little loss, Gone was the monopoly I had on her creation. She carried on the job of children; to grow and learn and become. Become a personality, an individual, an identity, a person. She found her voice, a beautiful husky utterance that I recognised as my own. We watched her stumble out her first steps and babble out her first words. Steps became skips and words became songs. She was blooming. And so was our love. And all this time, she had been observing, Drinking in language, gestures, concepts. Lapping up information and gathering opinions. Lots of them mine, but then, a word I do not say, or a gesture that is foreign. There is a dart of panic. A loss of control. An extension of the cord Now she is at school. Now the tables have turned. I am here for food, for clothes, for transport, for sleep. But there are many hours and many teachers and many friends, shaping my baby. This walking, talking, running, jumping, skipping, thinking, writing, reading; baby of my body. Then there are the moments before dawn, a little tip toe down the hall
There is a soft little voice and hand and she is curled in my body once again. Later, she will make her breakfast, dress herself, and run with friends But in this moment, rarer by the day, she has come home to rest. She is beautiful and she is mine. But when did she become apart from me? I will never know. And I will not hold her back. Though she may travel far and wide, She is my baby of my body, and always she will be. “But if my muscle is tight, why am I still leaking?” This is a great question. And the best way to answer it is to imagine we are talking about a different group of muscles in your body, such as your neck muscles. Most people will have experienced a sore and painful neck at some point in their life. And when you’ve had that sore neck, it’s often hard to turn your head, or you do so with trepidation, much more slowly than usual. Well, I bet during this uncomfortable time, you’ve also reached up to rub your sore neck and possibly touched the major muscle groups that are responsible for these neck movements. Did you ever notice how tight and hard they seemed under your fingertips? So, we have a sore neck, we have tight muscles and we have loss of function. This is exactly what is happening in your pelvic floor. Most often, something will have occurred in the pelvis to cause your pelvic floor muscles to became overactive and tight. This incident may have been, for example: a painful experience with constipation, a history of recurrent urinary tract infections or thrush, or an uncomfortable sexual experience. As a result, sometimes the pelvic floor muscles will go into spasm, or the individual may begin holding tension in the pelvic floor muscles as a way of subconsciously providing protection to the area. This causes the muscles to become short and stiffened. When muscles are held in a shortened position, they have less ability to contract and perform their function in a responsive and timely manner. If we go back to the example of our neck; turning your head (which is the function of the neck muscles), may be reduced, and will be performed more slowly in the presence of tight, stiff neck muscles. In the case of the pelvic floor, the ability to engage and contract to support the bladder and occlude the urethra (which is the function of the pelvic floor), will also be reduced, and will be performed more slowly when the muscles are tight and stiff, and this will lead to urinary leakage. So, if this is the case, asking this woman to do lots of pelvic floor exercises focused on squeezing and holding is not going to improve her urinary leaking. In fact, it may make it worse, or give her a new condition due to even more spasming in her pelvic floor muscles.
Instead, what will assist this woman is if she can learn to downtrain the muscle tension. This can be taught and practiced and once we have a healthy muscle, sitting at a good resting length, we can then teach appropriate functional recruitment of the pelvic floor which will lead to long lasting continence. I’m pretty much what you’d call a type ‘A’ personality. There’s a part of me that is, or used to be secretly proud of this statement. Doesn’t type ‘A’ mean you’re a perfectionist? That you work hard and achieve high? Well, maybe, but only if the conditions are perfect, and it’s likely that if you really are a type ‘A’ nothing will undo you’re perfect world faster than welcoming a little person or two into your life.
Type A’s like to have their ducks in a row, a very neat row. Generally, their brainwaves run at a pretty high velocity, often jumping on different thought trains and travelling fast in all sorts of directions. Sometimes helpful ones that solve problems quickly and get things done efficiently, especially if you can focus your full attention and can mobilise yourself to that task in that moment. But what happens when you are forced to slow down? When you cannot get off the couch because your 2 month old has decided they’ll only settle whilst on your chest but you know you need to get to the shops to make that dinner you had planned. Or when you cannot sit in front of the computer for 30mins to type that important email because you’ve just picked up the kids and they are hungry, need afternoon tea NOW, and need to tell you about a fight they had with a friend? What happens inside that type A mind? Does it accept this new state of incapacity? Of delay? Of imperfection? Or does it run faster? Does it try to do both things at once? The truth is being a parent sometimes (often) involves doing things well below your maximum brain power. So, it makes sense to do something else at the same time. Doesn’t it? I think about what I need at the shops while acting like I don’t know how to do a 9 piece puzzle with my 4 year old; I think about work and formulate a ‘to-do’ list while putting together a nutritionally balanced, interesting and hopefully palatable lunch box. I thought this was multitasking and patted myself on the back for proving to the invisible Gods that women can indeed do two things at once. However, as we learnt from last weeks blog, it’s not multitasking at all but instead a horrible state of mind called ‘Continuous Partial Attention’ which forces you into a constant state of adrenal attention and eventual chronic stress and has serious health impacts. For more on this, check out last week’s blog here. After years of doing this, I started to feel vague and disconnected. Like I wasn’t properly seeing or focusing on things. But more than that, it’s hard to describe…a sort of brain fog, a desensitisation, like an imposter was walking around in my life and they were doing a really bad acting job. It actually felt awful. Sometimes my days were passing, but I wasn’t noticing or enjoying them. And the odd thing was, I wasn’t being that effective, even though that was the whole point of multitasking in the first place. I’d start five different tasks, but not finish one. I’d think about abizzilion thoughts, but none of them would end anywhere useful or decisive. And all this while I was missing chunks of my day that left me feeling a bit powerless and lost. Then, I started hearing about the mindfulness movement, about being present, about immersing yourself in the sensations, the feelings and the thoughts of the present moment to achieve a calm and focused mental state. Yes! I thought. This is me…This is what I’ve been missing. I’ve been mentally somewhere else because I was trying so hard to be everywhere and be everything. I want to feel present all the time, I want to really see my kids when I look at them and hear their little voices. Not be caught up in some other task my brain is wanting to focus on. But it’s hard to do. The shopping list still needs to be thought about and doing the same 9 piece puzzle every day is mind numbingly easy. So how do we do it?! How do we genuinely engage in our present and not be temped into the easy trap of mentally drifting away? Well the first is to convince your brain that it’s not worth it. That doing several things at once does not in fact make you any more efficient. This may take some time because you’re brain is pretty stubborn, so you need to be patient, kind to yourself and persevere. Then, there are some pretty nifty Mindfulness tools you can use to bring your mind back to the moment. Here are some of my favourites: “One thing at a time.” When I feel my mind racing off in front of me, I rein it in by repeating “One thing at a time” to myself. It’s a great mantra and immediately forces me to be calm, methodical and see what is in front of me. Notice the small things. When my 4 year old is concentrating on a puzzle, she gets an adorable focused look on her face. I can see her brain ticking and her entire body is involved in locating the pieces, fitting them into place with her pudgy little fingers and then she gives herself an adorable clap when she’s done. When I focus on these details my mind is sharper, and alive. I feel happy that I’ve genuinely enjoyed watching this little piece of magic. Feel sensations on your skin If you are outside, become aware of the sun on your skin, or a cool breeze. If you are feeling warm and cosy or wearing something soft, take a few seconds to acknowledge the material sitting on your skin. Even better, if you are lucky enough to be holding a little persons hand, notice how soft it is, yet how much power they have to cling tight to you. Take a belly breath Breathing a full breath and travelling with the air into your nose, down your throat, into your lungs and through your blood and to your muscles is a great way of becoming aware of your body in the present. It also, floods your system with oxygen which rejuvenates your cells and gives your more energy. This is a good start. But it’s not an immediate fix. One thing I’ve learnt is that you need to forgive yourself. It’s helpful to treat your mind like you would a 2 year old. Steer it in the right direction, but when it starts playing up, gently, and with good humour, direct it back on task and don’t expect too much of it. Mindfulness, it’s a journey worth taking. Not one I profess to be much good at yet, but I really have no interest in continuing down the unfulfilling journey of poorly attempting to multitask, and I encourage you to do the same. I can’t do two things at once. Well, I can, sort of…but I’m trying to stop. You know why? It’s killing me. And I don’t just mean emotionally killing me, I mean it’s actually increasing my risk of cardiovascular disease, weight gain, osteoporosis and Alzheimer’s Disease….and that’s just the start of the list. I like being on top of things as much as the next person. I like being effective and feeling in control. So….I’ve been multitasking, or so I thought. Turns out what I thought was multitasking is actually something else coined Continuous Partial Attention (CPA) and it’s really bad for me. What’s the difference? Multitasking is literally doing two things at once, such as stirring pasta whilst having a conversation. But in order to really multitask, at least one of the tasks has to be so simple it is essentially automatic, in the above example it would be stirring the pasta. Continuous partial attention refers to doing two tasks that require cognitive attention at the same time. However, in actual fact, we are not performing the two tasks simultaneously, rather rapidly switching between the two, or three, or four, and this is where things begin to go drastically wrong… An example of CPA would be; following a recipe to make a new gluten-free, dairy-free, fructose-free dinner, whilst having two independent and unrelated conversations with a 7 year old and 4 year old, and receiving a text message… at the same time. The brain does not process these cognitive demands simultaneously, rather it’s doing a crazy aerobics workout reminiscent of a Les Mills Body Attack class and leaving you equally exhausted. This kind of shifting of concentration is driven by our desire to achieve across all levels, not to miss anything (I think the kids are calling it FOMO), and due to being chronically time-poor. Setting all the problems with these motivations aside for another blog on another day… let’s deal with the issue at hand, which is what impact is this constant CPA state having on our health? Continuous Partial Attention forces us to maintain our attention in a state of hyper-vigilance which in turn keeps our bodies’ flight-or-fight response activated. The flight-or-fight response is a natural, necessary reaction to a threatening or stressful situation that requires immediate action. It turbo charges our bodies for action and for repair, it mobilises stress hormones such as adrenalin and cortisol and increases platelet concentration and immune cells in preparation for tissue damage. It is designed to be used occasionally and for brief periods of time, such as running away from a lion. When it is chronically engaged, as in constant CPA, all these chemicals and physiological changes are being turned on, with nowhere to go. We experience this as anxiety. Image: Start running; an appropriate activation of the flight-or-fight response. This long term, over-activation of the stress response causes wear and tear on the body. Some of the symptoms are
Sooo…..who still thinks they’re being efficient when they’re multitasking? But it makes sense doesn’t it. Doesn’t it feel awful when you’ve been jittering around all day from unfinished task to unfinished task, never fully seeing or hearing the world (let alone your kids) around you? It did for me. And therefore, enter Mindfulness. But sorry, you’ll have to wait. This blog is long enough and I can’t possibly do justice to the force that is Mindfulness in less than 200 words. But I hope I’ve given you some food for thought. So don’t hold your breath for the next instalment, rather take a big belly breath and actively stop doing too many things at once, it’s really not good for you. Until next time. Kym So, confession time, I occasionally can be seen loitering in the ‘self help’ section of a book store. I actually find it fascinating, I am always sucked in to the opportunities for bettering my life and filled with an exciting sense that can only be described as “turning over a new leaf”. Here is the ‘self help’ section of my personal bookcase: (Oh, I feel a bit naked now!)
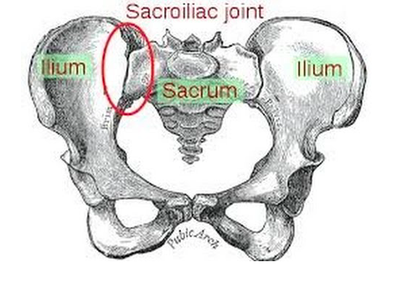
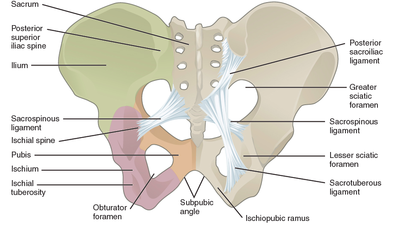
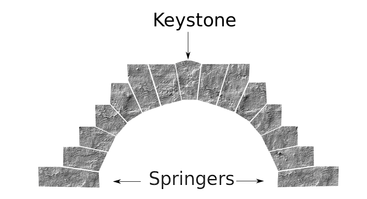
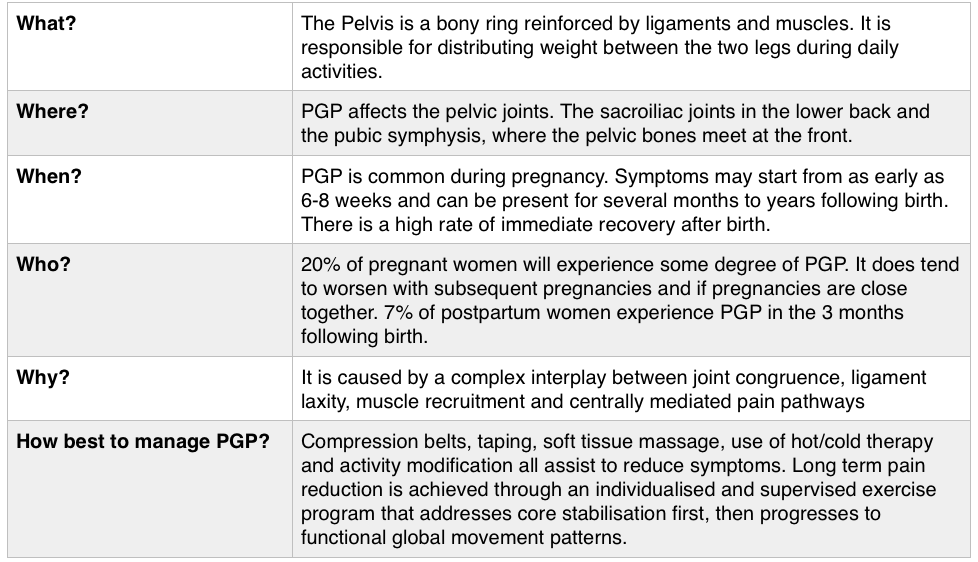
So, you may have spotted in my collection, Gary Chapman’s classic book ‘The 5 Love Languages’. For those of you who are not familiar with the 5 Love Languages, here they are listed below: -Words of Affirmation -Quality Time -Gifts -Acts of Service -Physical Touch The premise of the book is that most people identify with a particular love language and that is how they like to receive, and generally the default way that they give, love! So for example, If your love language is gifts, you like to buy people you love gifts, that is how you communicate your love. And generally, you expect gifts in return to feel loved. If your partner is speaking a different language, for example, is missing a night out with friends to be home with you watching a movie because his language is ‘Quality Time’, but you never get a look in, in his weekly shopping list, then we have a mismatch and fireworks can begin (the bad kind, not the good ones). Now I think I bought this book about 2 years into my relationship with my now husband, so no kids on the scene, not even a ring on the finger and still living separately. I distinctly remember identifying myself as a ‘Physical Touch’ linguist, I loved to feel the comfort of strong arms embracing me or the feel of his rough hands interlocked with mine as we walked down a street. My husband was a ‘Words of Affirmation’ kind of guy. This was interesting to us and fuelled a few good D&M’s (probably late at night over the cordless phones!) but I can’t recall there being much else to note. However, I do remember being very critical of the ‘Acts of Service’ language. Let me explain… Acts of Service refers to physically doing things for your partner as a way of showing you love them. For example, cleaning the house, mowing the lawn, taking out the rubbish, folding a load of washing. As a young independent woman in my early 20’s (who still lived at home and had very few responsibilities), I thought this was extremely mundane and old fashioned. How could anyone possible interpret that as passion? As an act of love? And what sort of person would you be if you expected that of someone you loved? I thought that meant you basically wanted a slave. I vowed never to speak that love language and proudly ticked the box ‘Physical Touch’ (so much more romantic!) Then, I moved out of home… And had kids…. Now; I would strip naked for a man who folds a load of my washing. Now; there is nothing sexier than my husband voluntarily cleaning up the kitchen and placing a fully cooked breakfast in front of me. Now, I get ‘Acts of Service’ as a love language. Oh boy, do I get it. And Physical Touch? Well, as a mum, I have been smothered, physically, for 7 and a half years. I have revelled in the softness of their skin, their pudgy arms clinging to my neck, their soft kisses all over my face, their little hands wrapped around my fingers. I regularly bury my face in their soft tummies to blow raspberries and they nudge their hard little heads under my chin and into my chest. I receive love through physical touch by the truckload, so I don’t actually need it from my husband. This paradigm shift in our relationship took a lot of figuring out (I’m making it sound easy here) and quite a while to get our heads around. The very rhythm of how we loved each other had to change as our needs changed. And between work, study, breastmilk, nappies, houses, kids and sleep deprivation it was hard to see things so clearly. But we got there, and lucky for me, now on a weekend morning…I get both my favourite love languages, hugs in bed with the kids while my husband cleans the kitchen and cooks breakfast! Now, you’re speaking my language! Kym. For resources and help with shifting your relationship after you have kids, check out this website: www.partnerstoparents.org If you are suffering or have suffered with pelvic girdle pain (PGP) you know the painful ache that permeates one side of your lower back when your walking or getting dressed, or the sharp grabbing pain at the pubic bone, that pulls you up short when you take that first step from the couch. It can come and go, it can swap sides, it will ruin your sleep, and it can prevent you from being that active, happy pregnant lady you always thought you’d be. Read on to answer all your questions about PGP and how best to manage it. (Note: If it gets too heavy, you can skip to the summary cheat sheet at the end ;)) What? The pelvis is a bony ring made up of the sacrum and the ilia bones meeting at the cartilaginous pubic symphysis at the front of the body. The bony structure is reinforced by active and passive structures, (muscles and ligaments/fascia), that contribute to its stability. The role of the pelvis is to allow movement, and to transfer and absorb forces between the trunk and the limbs. In an upright position, the weight of the head, arms and trunk are transferred to the lower limbs through the sacrum, the sacro-iliac joints, the ilia bones, and into the femurs. For load to be smoothly transferred, movement at the sacroiliac joints must be minimised. The body does this in two ways: form closure and force closure. Form closure refers to the anatomical shape of the bones and the complimentary joint surfaces that cause the sacrum to form a keystone effect between the two ilia bones. During weight bearing the sacrum is forced downwards and tilts slightly forward (this is caused nutation). This causes a close-packed position of the sacroiliac joint and contributes to stability and efficient weight transfer. Force closure refers to ligaments, muscles and fascia that work across the joint to further compress and stabilise the bony surfaces. Nutation of the sacrum causes tightening of the sacroiliac ligaments. Muscles that cross the joint, (namely piriformis and gluteus maximus) will activate to provide additional stability. Additionally, studies have demonstrated that transverse abdominus, the inner-most abdominal muscle, contributes to stabilising the lower spine and the sacroiliac joints (Hodges, 1999). Where? PGP is described as pain experienced between the posterior iliac crest (top of the pelvis bone at the back) and the gluteal fold (the crease where your bottom finishes and your leg begins), predominantly at the level of the sacroiliac joints with or without referral into the back of the thigh. Pain can also be experienced in conjunction with, or exclusively in the pubic symphysis (the bone between your legs at the front). When? PGP can occur at anytime, but most commonly presents during pregnancy or postpartum. During pregnancy, the expanding and increasing weight of the uterus puts a biomechanical strain on the body, in particular the lumbar spine and the pelvis. The load on local tissues causes creep (gradual stretch), which may contribute to stimulation of mechanoreceptors inducing increased activation of pain receptors. Creep also has implications for a change in proprioception (knowing where the body is in space), and therefore motor control, which means the brain’s ability to activate and control muscle sequences for optimal movement. Additionally, the growing abdomen during pregnancy leads to a change in the angle of pull of the deep abdominals, making them less effective for stabilising the sacroiliac joint. Pregnancy comes with an increase in the hormones; relaxin, oestrogen and progesterone, which contribute to increased soft tissue laxity. The contribution toward PGP each of these hormones makes is still unclear. A systematic review of the literature in 2012, looked at the relationship between relaxin levels and pelvic girdle pain in pregnancy. Three of the four high quality studies, found no association between relaxin levels and the presence of pelvic girdle pain. In other words, despite documented high levels of hormones and increased joint laxity, this does not always correlate with the presence of PGP. Who? PGP is common during pregnancy, prevalence data from large studies show an agreed prevalence in a pregnant population of 20%. The recovery rate of PGP following pregnancy is high, with one study of 41,241 women reporting an 82.5% recovery rate in women who experienced pain during pregnancy. The overall prevalence of PGP experienced in the first three months postpartum is reported as 7%. The literature agrees that a more severe pain experience involving more than one pelvic joint during pregnancy is associated with an increased likelihood of PGP postpartum. Pregnancy and new parenthood is a time of great life-change, and brings stressors that are foreign and can seem insurmountable. Post-natal depression affects one in seven women and the ‘baby blues’ affects approximately 80% of new mothers. A lesser known condition is ante-natal depression which occurs during pregnancy and affects 10% of women (PANDA). Additionally, sleep deprivation to varying degrees impacts all new parents. Sleep deprivation has been found to cause hyperalgesic changes in the body, which contribute to chronic pain. PGP must be approached within a biopsychosocial framework. Pain is influenced by cognitive and psychosocial factors that modulate pain amplification and disability levels. It is known that ongoing pain can be centrally mediated by the forebrain, it is therefore understandable that PGP disorders can potentially be induced and /or maintained through a balance of peripheral physiological mal-adaptive behaviours, and centrally mediated pain sensitisation. Why? Putting all the who, what, where, and when together brings us to the why? So, we know the sacroiliac joint requires stability to function, that is, to transfer weight efficiently and pain-free from one leg to another. Factors that reduce this in pregnancy are increased ligament laxity, decreased efficiency of muscle activation through altered proprioception and motor control, and in the case of abdominals, less efficient angle of pull. Combine this with an increased load to transfer as the uterus expands with the growing foetus and the pelvis has it’s work cut out. However, still only one in five women will experience pelvic girdle pain. So, why? Well joint stability is not about how resistant structures are to movement or how much movement is available but instead, about the motion control that allows load to be transferred and movement to be smooth, effortless and painfree (Vleeming et al., 2008). Meaning, that it is the complex interplay between these factors that combine to present as pain. How is PGP managed? Physiotherapists have many tools that we use to reduce pelvic girdle pain, these include: -External Pelvic Compression with Belts/Tape/Compression garments -Soft Tissue Mobilisation -Hot/Cold Therapy -Activity Modification/Education -A Specific and Individualised Exercise Program. Accurate movement analysis and postural assessment is essential to long term recovery. Many studies have analysed exercise regimes; common theories are Vleeming’s anterior/oblique, posterior and vertical muscular slings. Or the functional activation pattern initially proposed by Stuge and her team in 2004 which begins with strengthening local stabilising muscles such as transverse abdominus, pelvic floor and multifidus prior to building in more global stabilisers such as latissimus dorsi, gluteus maximus, abdominal obliques and hip adductors and abductors. Results vary between studies, but there is a trend in the literature to support individualised, exercise prescription that emphasises deep stabilising muscle activation, and functional progression received one-to-one by physiotherapists over at least 6 weeks. It can be concluded that global muscles alone, despite ability to increase stability of the SIJ, have no impact and may potentially exacerbate symptoms if not recruited in an activation pattern that includes local core stabilisers of the lumbo-pelvic region as well. Supervision of exercises is important to ensure quality of exercise performance and to translate to pain reduction. Summary (the cheat sheet): Whether you have symptoms of PGP, have had symptoms, or are a health practitioner who see’s patients with PGP, I hope you got something out of this information that will help you. I practice women’s health physio in Lower Plenty, Melbourne and regularly care for women with acute and chronic PGP. I am always happy to chat and share information, so feel free to make contact with me at any time. Kym References: Albert H, Godskesen M, Westergaard J (2001) Prognosis in four syndromes of pregnancy-related pelvic pain. Acta Obstet Gynecol Scand 80:505–510 Heckman JD & Sassard R (1994) Musculoskeletal considerations in pregnancy. Journal of Bone and Joint Surgery American Volume 76, 1720–1730. Hodges PW (1999) Is there a role for transversus abdominis in lumbo-pelvic stability? Manual Therapy 4, 74–86. Lautenbacher, S., Kundermann, B., Krieg, J. (2006). Sleep deprivation and pain perception. Sleep Medicine Reviews. 10(5): 357-369. Lillios, S., Young, J. (2012). The Effects of Core and Lower Extremity Strengtheinin on Pregnancy-Related Low Back and Pelvic Girdle Pain: A Systematic Review. Journal of Women’s Health Physical Therapy. 36(3): 116-124. Marnach, M., Ramin, K., Ramsey, P., Song, S., Stensland, J., An, K. (2003). Characterization of the relationship between joint laxity and maternal hormones in pregnancy. Obstetrics and Gynecology. 101(2): 331-335. Ostgaard, H., Zetherstrom, G., Roos-Hansson, E., Svanberg, B. (1994b). Reduction of back and posterior pelvic pain in pregnancy. Spine. 21:2777-2780. Pennick, V., Liddle, S. (2013). Interventions for preventing and treating pelvic and back pain in pregnancy. Cochrane Database of Systematic Reviews. 8. Schauberger, C., Rooney, B., Goldsmith, L., Shenton, D., Silva, P., Schaper, A. (1996). Peripheral joint laxity increases in pregnancy but does not correlate with serum relaxin levels. American Journal of Obstetrics and Gynecology. 174: 667-71. Stuge, B., Veered, MB., Laerum, E. et al. (2004). The efficacy of a treatment program focusing on specific stabilising exercises for pelvic girdle pain after pregnancy: a two-year follow up of a randomised clinical trial. Spine. 29:197-203. Vleeming, A., Stoeckart, R., Volkers, A., Snijders, C. (1990). Relation between form and function in the sacroiliac joint. Part 1. Clinial anatomical aspects. Spine. 15: 130-132. Vleeming, A., Volkers, A., Snijders, C., Stoeckart, C. (1990b). Relation between form and function in the sacroiliac joint. Part 2. Biomechanical aspects. Spine. 15:133-136. Vleeming et al. (2008). European Guidelines for the diagnosis and treatment of pelvic girdle pain. Spine. 17:794-819. Vermani, E., Mittal, R., Weeks, A. (2010). Pelvic Girdle Pain and Low Back Pain in Pregnancy: A Review. Pain Practice. 10(1): 60-71. Last night, while the kids were in the bath, my husband was being a goofball and popping out from behind a door making funny faces, causing them to shriek with adorable, bubbling laughter. I was sitting in our bedroom, folding the washing and enjoying the spectacle. He came into the bedroom and while we were chatting he commented that he thinks a lot about the legacy he will leave as a father.
My immediate thought was ‘that is really good!’ Of course I want the father of my children being aware of the impact he is leaving on our kids. This thought was quickly followed by another…. “I don’t think about the legacy I’m leaving on our kids a whole lot” Whoops. I mean, I should be, right? I did when I was pregnant, I even wrote down the sort of mother I wanted to be. My notes were filled with good intentions, to create a happy home filled with love, security and acceptance of my children and whatever they wanted to be. I also (now I realise, stupidly) wrote down little details about how my children would behave, like I had a choice or could hope to mould them so clearly. But time for those dreams is a thing of the past. Time to wistfully imagine my perfectly endless compassion and patience as a mother does not factor into my day to day, real life actual mothering. Now, don’t get me wrong its not that I don’t still want all that, but do I actually achieve that daily? I’m not sure. It’s hard to think about it or assess it between getting everyone dressed and fed, doing hair, and packing the dishwasher for the 3rd time that day. So, what will be my legacy? As I was sitting there, methodically sorting and folding the washing with a careful eye on my girls playing in the bath, I took a breath (shout out to my meditation teacher Cath Guilesspie for that little lifesaving tip!). And that helped me to step off the perfectionist panic train in my brain. I realised what my legacy will be. It will be being there. And now stop, I don’t mean that in any amazing, betty home-maker, always mindfully present kind of way. Cos that’s not me, at all. But I definitely always go and check on them after the 5th time they call out, or when the crying really escalates to the point that I’m worried the neighbours might complain, or if there’s blood. I’m always prompt if there’s blood. No seriously, I really mean, just being human and doing it in front of them. Like making mistakes, like crying, like dancing a little crazy to ‘shake it off’ or belting out Adele’s “Hello” while they watch in a mystified horror. Like having an argument with my husband and then finding a resolution, showing them it’s ok to have a strong opinion and stand up for it, and also the importance of understanding and compromising. They are watching me devote time to building my business, learning the importance of hard work and doing something you believe in. They see my husband and I commit to sports and sometimes that means, time away from home but I hope they are learning the value of staying active and getting involved. Legacy will be what it will be, it is not generated in a day, or a week. It is the sum of all your actions. And no amount of diary writing or wishful thinking will probably impact it. It’s nice to think about it occasionally and do a little assessment of how I’m tracking, but at the end of the day, being there and being human, the good and the bad, will demonstrate the greatest strength and is the best legacy I can leave behind. Phew! xx So, I do Crossfit. And I’m a pelvic floor physiotherapist. If you haven’t heard….these two things combined are a little controversial. When Crossfit made and released the below video, I am sure they did not anticipate the barrage of criticism that was unleashed by hundreds of enraged continence physio’s worldwide. We can be a passionate bunch….we normally only need a little poke to get started, but this was like waving a red flag at a bull. So much material to tear apart! And they couldn’t have made it easier…….Geez, they started by calling the medical condition by the wrong name! So, enough talking - if you haven’t seen it, here it is: Crazy? Yes. Appalling? Indeed. Now, as I referred to before, there has been a barrage of well articulated articles written by pelvic floor health professionals about everything that is wrong with this clip. Here are two of the best which I encourage you to read: http://physiodetective.com/2013/06/27/crossfit-your-pelvic-floor-and-peeing-during-workouts/ https://pelvicguru.com/2013/06/22/dear-crossfit-and-crossfit-gynecologist-im-appalled-theres-help-for-peeing-during-workouts/ But, despite all this….I still do Crossfit. And here’s why:
So, what about the pelvic floor? Well, Stress Urinary Incontinence (which is the internationally accepted correct terminology) occurs when the intra-abdominal pressure above the bladder exceeds the closure pressure generated by the pelvic floor muscles and soft tissue structures below the bladder. This pressure can come from weight, from impact caused by the ground reaction force, and by bracing the abdominals. The thing is, yes these things can occur during Crossfit, but they also occur during Netball, Tennis, Soccer, Football, Dancing, Running, Jumping on the trampoline and any other activity that involves pushing your body. Should we accept it if we leak during ANY of these activities? No. And that’s where The Crossfit clip went so terribly wrong. Don’t accept it, treat your incontinence as you would treat any injury in your body - don’t push through it, get it assessed, scale back until you can do the movement with correct technique and no dysfunction, which in the case of the pelvic floor muscles, means no urinary leaking or feelings of heaviness. If you are thinking about starting Crossfit, research your choices. Choose a box that has experienced coaches, has an induction training program, that limits class sizes so technique can be monitored, and that doesn’t pressure you to add weight or intensity unless you are ready. If you are concerned about your pelvic floor function or don’t know how to control your pelvic floor muscles, make an appointment with a pelvic floor and continence physio who can answer all your questions or visit my website at womankindphysiotherapy.com. Enjoy your WOD! |
Welcome!Hi! Welcome to The Blog! Please be aware, Womankind Physiotherapy's blog is not intended to replace information and advice from your health care provider. For specific concerns regarding your health you must seek individualised care by your preferred provider.
Archives
March 2021
Categories
All
|
Women's Health Physiotherapists, Pelvic Floor Physiotherapists, Pregnancy Physiotherapists, Pre and Post Natal Physio, Pelvic Health Physio,
Pregnancy Pilates, Ultrasound for Mastitis, Breastfeeding Physio, Blocked Ducts, Pelvic Floor Exercise, Pregnancy Exercise.
Eltham. Yarrambat. Greensborough, Montmorency, Lower Plenty, Diamond Creek, Research, Rosanna, Yallambie, Watsonia.
Pregnancy Pilates, Ultrasound for Mastitis, Breastfeeding Physio, Blocked Ducts, Pelvic Floor Exercise, Pregnancy Exercise.
Eltham. Yarrambat. Greensborough, Montmorency, Lower Plenty, Diamond Creek, Research, Rosanna, Yallambie, Watsonia.
Copyright 2016 Womankind Physiotherapy


















 RSS Feed
RSS Feed